Patient Involvement, Engagement and Empowerment
There is substantial evidence that patient involvement, engagement and empowerment have the potential to improve not only patient satisfaction with care but also the quality of care provided, and also improve patient outcomes (83). In such activities, patients and healthcare professionals work in equal partnership to promote and support patients’ active involvement in advancing their health and healthcare and also research and innovation. ‘Engagement’ expresses the commitment and actions of healthcare professionals to include patients in discussions and decisions about their care as individuals and in the development (‘coproduction’) of plans for healthcare services and research. ‘Empowerment’ is a wider, more complex concept that encompasses commitment and action by patients that are self-derived and self-driven and may occur outside the interactions with healthcare professionals. ‘Engagement’ and ‘empowerment’ overlap, interact and strengthen each other. The degree of empowerment or engagement that is desirable for an individual depends on the person’s preferences and experience. The aim is to ensure that care delivery is always responsive to people’s physical, emotional, social, and cultural needs. Staff interactions with patients are empathetic and informative. The patient’s personal values and preferences are elicited and acted upon (83-85).
The European Patients’ Forum (EPF) defines empowerment as a ‘process that helps people gain control over their own lives and increases their capacity to act on issues that they themselves define as important’. EPF has developed a Charter on Patient Empowerment which characterizes an empowered patient (Figure 8, 84). Shared Decision Making (SDM) is a key feature of good care and patient engagement and is discussed further under The Code 6.
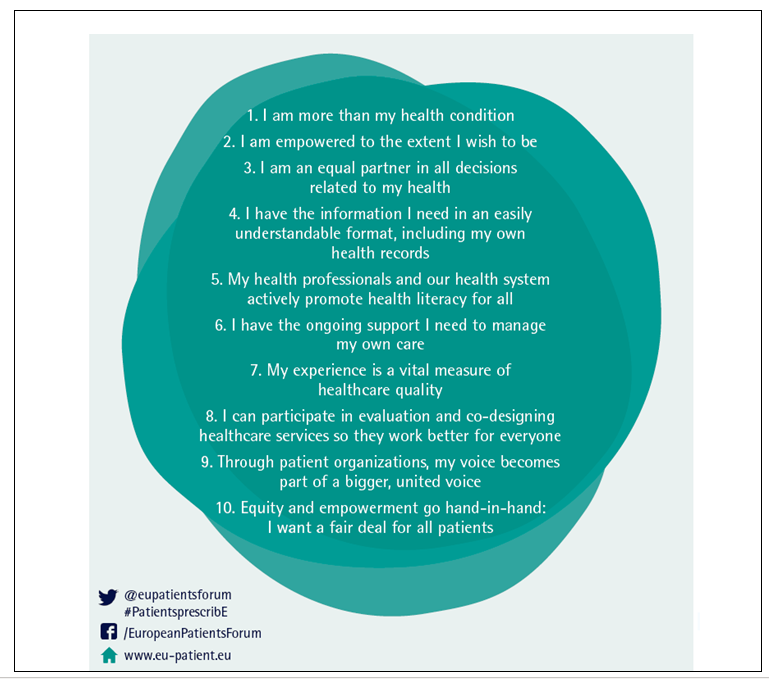
Figure 8. The EPF Charter on Patient Empowerment (84)
Despite growing acceptance of the concept of patient empowerment, uncertainty still exists about how we can measure it. Systematic reviews of scales that measure empowerment exist (86), drawing on a range of related concepts (83-86), the most relevant being:
• self-efficacy (the strength of a person’s belief in their ability to succeed in accomplishing a goal, task or challenge)
• locus of control (how far a person is inclined to see what happens to them as being mostly under the control of external factors or largely under their own control)
• health orientation, which sets out to measure whether and how far an individual is motivated to engage in healthy behaviours and take responsibility for their own health
• health literacy, which is the extent to which an individual has the capacity to obtain, process and understand health information and services on which they can make appropriate health decisions
The goals of patient involvement, engagement and empowerment include improved patient outcomes, ie improved QoL and well-being; enhanced adaptation to the long-term effects of treatments; greater independence from healthcare providers and carers; and more effective and sustainable healthcare systems. Patient involvement, engagement and empowerment are ethical imperatives and a rational and evidence-based choice, resulting in better psychosocial and economic health outcomes (83-86). Venetis et al (87) found that when patients felt they were being listened to, they felt more valued, more positive and more satisfied, and they reported increased confidence and fulfilment. Individuals may subsequently experience greater control over their illness, improved treatment outcomes and reduced anxiety; they are thus healthier and enjoy better QoL. Active patients may comply and manage care better, thereby easing healthcare economic constraints. There is increasing acceptance that in planning cancer services and in the education of healthcare professionals, we should stress the benefits that can flow from active engagement of patients in their care (83-88).
Back to Medical Literature and Evidence for the European Code of Cancer Practice


